The bradycardia algorithm lists the proper sequence used to treat a patient with symptomatic bradycardia with a pulse. Bradycardia is associated with a slow heartbeat. Although individuals, such as well-trained athletes, may have a resting heart rate of 40–50 beats per minute without any symptoms, it is crucial to identify the differences between symptomatic and asymptomatic bradycardia.
Symptomatic bradycardia is necessary to differentiate symptoms resulting from the low heart rate from those that are unrelated. Read more about ACLS bradycardia algorithm below.
What is bradycardia?
An adult’s heart rate must be between 60 and 100 bpm. Bradycardia means slow heart condition in Greek and occurs when the heart beats slower than expected. Although the condition can be asymptomatic, it prevents the heart from supplying adequate oxygen-filled blood to the body.
A human heart comprises four chambers that are divided into two distinct parts, known as the atria and ventricles. The right atrium comprises the sinus node and controls the heart’s rhythm via electrical impulses. These cause the atria to contract while pushing blood to the ventricles. This travels to a cluster of cells known as the atrioventricular (AV) node. The AV node sends signals to a collection of cells, causing the ventricles to contract and send blood to other parts of the body.
Bradycardia takes place when electrical impulses are blocked. Issues with irregular heart rhythm originate in the sinus node, as it is the natural pacemaker of the body. Blockages between the atria and ventricles may prevent impulses from traveling from one chamber to the other.
What are the common symptoms of bradycardia?
- Dyspnea
- Fatigue
- Syncope or near syncope
- Lightheadedness or dizziness
- Chest pressure, heaviness, and pain
- Dyspnea
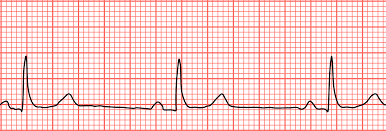
What are the ECG rhythms you must know to treat bradycardia?
- Sinus bradycardia
- Second-degree AV block
- Second-degree AV block
- Type 1 (Wenckebach phenomenon/Mobitz I)
- Type II (Non-Wenckebach/Mobitz II)
- Third-degree AV Block
Once you have identified symptomatic bradycardia, identify and treat the underlying cause, and use the H’s and T’s of ACLS to help with this step. You must maintain the airway and assist in breathing. Then administer oxygen if hypoxemic. Monitor blood pressure, connect a cardiac catheter, and establish IV access. When a 12-lead ECG is available, utilize it. However, do not delay in obtaining one. The next step involves assessing if the patient shows adequate perfusion.
What are the common signs of persistent bradycardia causing poor perfusion?
- Signs of shock
- Chest discomfort
- Acutely altered mental status
- Acute heart failure
- Hypotension
Observe and monitor if the perfusion appears adequate. If the patient is showing the above signs that indicate poor perfusion, go forward to the next step and administer atropine. If atropine is ineffective, administer epinephrine or dopamine or transcutaneous pacing.
How to diagnose and treat bradycardia?
Bradycardia may occur without symptoms. The diagnosis of bradycardia requires that the patient have a heartbeat less than 60 bpm and have symptoms. According to the ACLS provider manual, here are the symptoms included:
- Increased capillary refill time
- Pale and cool skin
- Diminished or absent peripheral pulses
- Heart rate: <60 bpm
- Distressed respiration, which may progress to respiratory failure
- Decreased capillary refill time
- Fatigue or dizziness
How do you assess and manage the patient using primary and secondary surveys?
Start by identifying the cause while preparing the patient for treatment. Provide breathing assistance, maintain the patient’s airway, and monitor heart rate and blood pressure while establishing IV access. Follow the procedure by reviewing the heart rhythm of the patient and obtaining a 12-lead electrocardiogram (ECG). Administer oxygen whenever required and complete an examination.
Assess the adequacy of perfusion. Next, determine if there is adequate perfusion. Check whether the patient is showing signs of an altered mental state, such as chest pain, hypertension, or heart failure. Monitor and observe, if they aren’t.
Consider applying atropine when IV access is available. Use this repeatedly, up to six doses, or 3 mg, every 3 to 5 minutes. Start pacing where the application of atropine is not adequate.
If there are signs of severely poor perfusion, then do not delay pacing to administer atropine. Start TCP at a rate of 60/min. Feel free to adjust as per your requirements. Check the response with the help of a femoral pulse instead of a carotid pulse, as muscle movements might affect the latter. Use dopamine (2 to 20 µg/kg each min) or epinephrine (2 to 10 µg/kg each min), where the pacing is insufficient. Enact these actions in rapid succession and prevent cardiac arrest.
Conclusion
Thus, the ACLS bradycardia algorithm helps us learn how to treat a patient with symptomatic bradycardia. Assess the symptoms, know the causes, and treat them with the help of the steps mentioned above. Follow this step-by-step description of adult bradycardia as mentioned above.